Type 2 Diabetes Mellitus (T2DM) affects more than 37 million Americans, and it can be a serious condition if left untreated. Let’s take a closer look at some of the causes, symptoms to look out for, and how you can take care of yourself if you do develop T2DM.
What is Type 2 Diabetes Mellitus (T2DM)?
Type 2 Diabetes Mellitus (T2DM) — also known as type 2 diabetes, non-insulin-dependent diabetes, TDM, or T2D — is a long-term, chronic condition in which your body becomes unable to properly regulate sugar levels in the blood. This causes a wide range of unpleasant symptoms and, if left untreated, can lead to severe or even life-threatening complications.
When you eat, you ingest a type of sugar called glucose. As glucose moves through your body, your pancreas creates a hormone called insulin that regulates how much glucose is absorbed by your cells. When a healthy amount of glucose enters your cells, they can produce energy.
T2D occurs when your cells become resistant to insulin and are therefore unable to properly use it. In response, your pancreas produces more and more insulin to try to trigger the cells to do their job. Because of this insulin-resistance, the glucose you consume goes into your cells unregulated, and your glucose rises to unhealthy levels.
What Are the Symptoms of Type 2 Diabetes?
If you’re at risk of developing type 2 diabetes, it’s helpful to know what might be signs of symptoms of the condition. Some of the most common early symptoms of T2DM include:
- Extreme thirst
- Chronic fatigue
- Sudden and unexpected weight loss
- Frequent urination
- Constant hunger
- Vision is or becomes blurry
- Unusually slow healing of skin wounds
- Excessively dry skin
- Numbness or tingling in the hands and/or feet
- Frequent headaches
- Bleeding gums
- Darkened skin around the armpits and neck
Women who have T2D may also experience frequent yeast infections or urinary tract infections. Polycystic Ovary Syndrome, or PCOS, is also related to T2D. Women who have PCOS or a family history of PCOS are more likely to develop T2D.
Two symptoms particular to men with T2D include erectile dysfunction and decreased muscle mass.
For children, they may show any of the above symptoms, but the most common are extreme thirst, chronic fatigue, blurry vision, and increased urination.
Some symptoms of diabetes may take years to appear, and some people may be completely asymptomatic. It’s important to get regular blood tests to monitor your glucose levels and determine if you’re at risk of developing diabetes.
What’s the Difference Between Type 1 and Type 2 Diabetes?
Both types of diabetes are caused by the body’s inability to regulate insulin. However, there are several important differences between type 1 and type 2 diabetes.
With T1D, your pancreas is unable to make insulin. With T2D, your pancreas is able to make insulin, but your body is unable to use it correctly. People who have T1D need to take insulin, while people with T2D may or may not need to take insulin.
Age
Type 1 diabetes is still sometimes called “juvenile diabetes” because it is most commonly diagnosed in children and teens. Type 2 diabetes can occur in children and teens, but has historically been called “adult-onset diabetes” because it is most commonly diagnosed in adults.
Causes
T1D is believed to be caused by an autoimmune disease in which the body’s immune system attacks its own insulin-producing cells inside the pancreas. T1D tends to run in families.
T2D, on the other hand, is caused by several factors. Some of these factors are related to lifestyle, while others are genetic.
What is the Leading Cause of Type 2 Diabetes?
There are many known factors that could contribute to T2D:
- Obesity, especially excessive belly fat
- A sedentary lifestyle
- Over 40 years old
- High blood pressure
- A history of gestational diabetes for those who have been pregnant
- A history of giving birth to one or more babies weighing over 9 pounds
- Low levels of “good” cholesterol (HDL)
- A diet heavy in processed food and sugar
- Being ethnically Black, Latinx, Native American, or AAPI
- Having a 1st degree relative with T2DM (parent, sibling, or child)
- Untreated pre-diabetes
- Polycystic Ovary Syndrome (PCOS)
- Stress
Exhibiting one or more of these risk factors isn’t automatically a sign that you have diabetes. Always ask your doctor if you have questions or concerns about your experiences or your lifestyle.
Of these factors, obesity is considered the leading cause of type 2 diabetes.
How Does Obesity Cause Type 2 Diabetes?
Obesity by itself does not cause T2D, and not everyone who qualifies as obese will develop T2D. However, there are strong links between obesity and T2D. Obese adults may be up to ten times more likely to develop T2D than their non-obese peers.
Excess weight prevents your body’s cells from reacting to insulin properly. This leads to insulin resistance. When your body can’t properly use or react to insulin, too much sugar is left in the blood, and this excess can lead to the development of diabetes. Extra glucose is usually stored in the liver, but when someone carries too much weight, their fat cells prevent the liver from doing its job. The pancreas then works harder to make more insulin, which wears down the pancreas.
What Are the Possible Complications of Type 2 Diabetes?
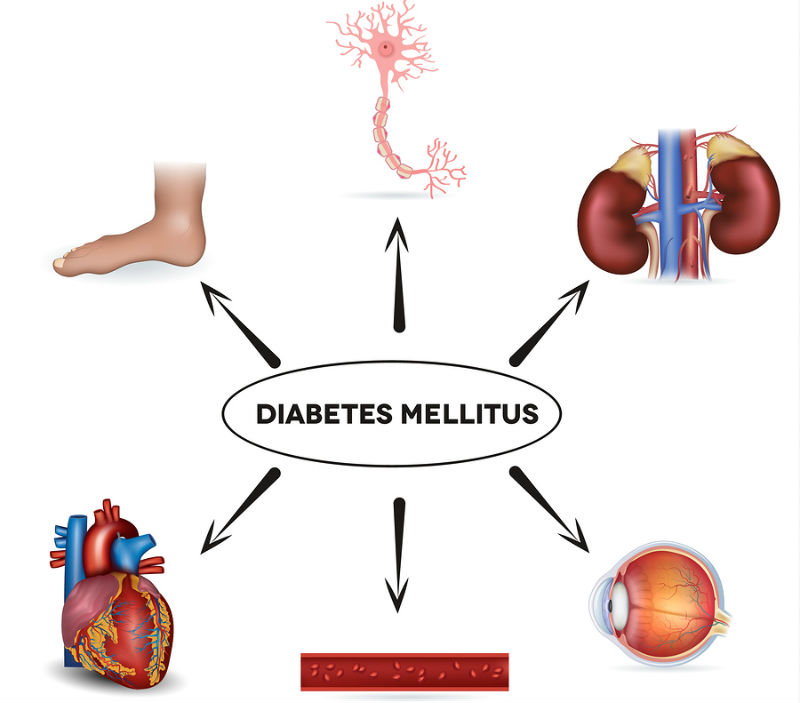
Left untreated, type 2 diabetes can lead to an increased risk of heart disease or stroke, sexual dysfunction, miscarriage or stillbirth, nerve damage that may require amputation (especially in the feet), permanent eye damage, and chronic kidney disease. If continued to be left untreated, these T2D-related complications can cause premature death.
T2DM Treatment
While there is currently no cure for either type of diabetes, there are lifestyle changes and other treatments you can utilize to manage your T2DM.
Monitor Your Blood Sugar
If you have been diagnosed with T2D (or even if you’re pre-diabetic), it’s crucial to regularly monitor your blood sugar levels so you can stay within your target range. Your doctor can help you determine this range, as well as what to do if your levels get too high.
Medications
Some types of diabetes require medication to help you maintain your target blood sugar levels. Depending on your initial diagnosis and glucose levels, your doctor may prescribe insulin to help your body manage blood sugar levels. Insulin may be prescribed as a first-step treatment, or if other medications, diet, and exercise aren’t helping.
Exercise
Some exercise is better than no exercise, but aim for about 30 minutes at least 4 days a week. You don’t need to exercise for 30 minutes all at once. And you don’t need to strain yourself. A few brisk walks throughout your day can make a big difference. It’s worth noting that muscle cells use extra glucose more efficiently than fat cells and can help reduce high blood sugar levels.
Diet
Reduce the amount of processed food you eat. Limit your intake of carbohydrates and simple sugars. Avoiding sugary drinks and incorporating more low-fat dairy products, green leafy vegetables, whole grains, beans, and nuts can help reduce your risk for diabetes, and they’re part of an overall healthy diet.
Plus, if you’re a coffee fan, you’re in luck. Drinking 2-3, 8 oz. cups of coffee per day can decrease your risk of diabetes by 11%.
Find healthy recipes that are fun to make and delicious to eat so you’ll be more likely to stick with your diet.
Weight Management
The combination of a better diet and increased exercise should help you lose weight. Losing just 5-10% of your body weight can greatly improve your body’s ability to absorb insulin and manage your blood sugar levels. You’ll notice a decrease in your diabetes symptoms and you’ll reduce the risk of serious complications. Once you’ve lost a certain amount of weight, your doctor may even take you off medications.
If you’re having trouble losing weight on your own, you may consider bariatric surgery. It’s worth asking your doctor if you qualify.
How Barix Can Guide You on Your Weight Loss Journey
While losing weight is one of the best ways to manage your type 2 diabetes mellitus, it’s not always easy. Even if you do lose weight, it might not be enough. That’s why the doctors at Barix Clinics are here to help!
Bariatric surgery is a safe and effective way to lose weight and get control of your life. Over 50,000 patients have had successful bariatric surgery with Barix Clinics, including some who have improved their T2D! Barix Clinics are about more than surgery. The teams at Barix will help you make lifestyle and diet changes so you can live the life you deserve.
Contact Barix Clinics today for a consultation and to find out how our team of caring doctors can help you start your new life.